Supporting Young People with ARFID: Why One Size Doesn’t Fit All
For parents and carers of children with ARFID (Avoidant/Restrictive Food Intake Disorder) or ARFID traits, knowing how best to help can feel overwhelming. At First Steps ED, we understand that every young person is different, and there isn’t a single approach that works for all. The support we offer is flexible, creative, and tailored to each child’s individual needs, with dedicated pathways for those experiencing ARFID.
Understanding ARFID and Neurodivergence
ARFID is often linked to sensory sensitivities, fear of new foods, and strong preferences for specific tastes, textures, and smells. It may also involve a lack of hunger cues or general disinterest in food and eating. Many of the children we support are also neurodivergent – over a third of our service users have neurodivergent conditions, with research suggesting that 4–23% of people with eating disorders may be autistic. These overlaps mean that traditional eating disorder treatments aren’t always the right fit, which is why our ARFID support draws on CBTAR (Cognitive Behavioural Therapy – ARFID) principles while remaining adaptable, gentle, and person-centred.

At First Steps ED, we take the time to understand each child’s individual experiences. Our Specialist Support Officers work collaboratively with children and families to explore sensory triggers, reduce food-related anxiety, and build confidence around eating in a way that feels safe and achievable. This personalised approach is central to how we support ARFID, ensuring that the child’s unique needs guide the pace and direction of their journey.
Creative, Person-Centred Approaches
At First Steps ED, we use a range of creative techniques to help children explore food in ways that feel safe, engaging, and fun. Some examples include:
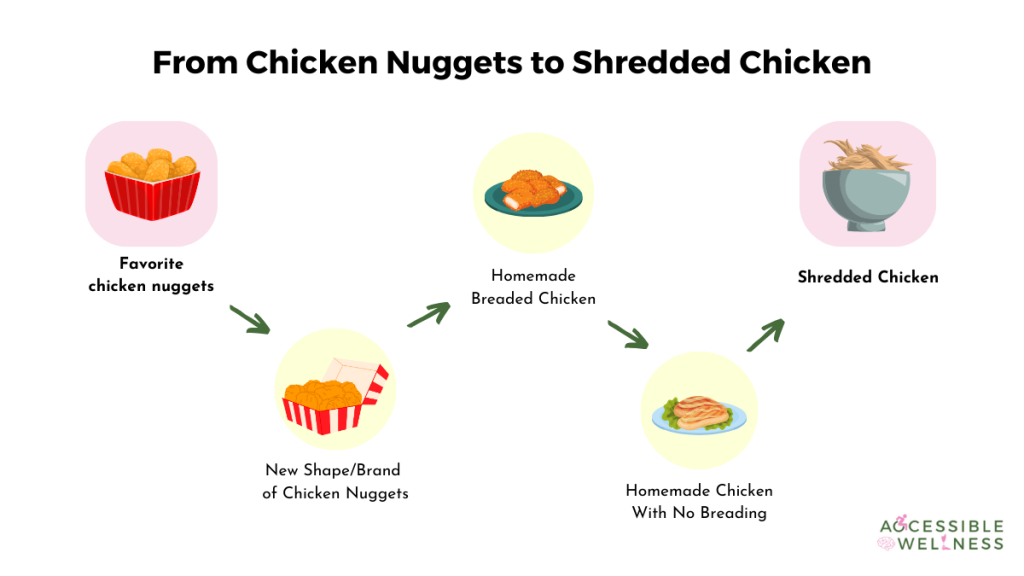
Food Chaining
Food chaining is a gentle, structured approach often used to support children with ARFID. It works by helping them move from foods that already feel safe to new foods with similar characteristics. Instead of asking a child to try something completely unfamiliar, we build a “chain” of related foods, each step only slightly different from the last.
For example, if a child comfortably eats crispy chicken nuggets, the next link in the chain might be a similar brand, then a homemade version, then a lightly seasoned piece of chicken. Each step feels manageable because the food still looks, smells, or feels familiar. This also leads onto a key part of our support – graded exposure, which includes having a new food on the table, on the child’s plate, feeling the texture, without the expectation to eat it immediately.
Externalising ARFID
Drawing ARFID as a character, monster, or “gremlin” helps children separate the disorder from themselves. We explore together what the ARFID needs to feel calmer, as a result, helping the child feel ready to try new foods once they are regulated.
Sometimes, the young person may find it useful to create an “alien” visiting Earth, giving the alien its own personality and voice. Food becomes a “new object” that the alien is curious to try, reducing anxiety and fear responses. Sensory exploration (sight, touch, smell, taste) is done gradually, without pressure to eat, fostering curiosity rather than stress.

Creative Projects Inspired by Interests
One of our service users designed packaging for a new food, focusing on mindful eating and describing what the food was like; another created a radio jingle to advertise a food, combining music, performance, and play.
Special interests, like Mario Kart or Pokémon, can also be woven into sessions to spark engagement. One service user wanted to explore the food she saw from watching the film K-pop Demon Hunters, which gradually built her up to trying sushi and ramen.




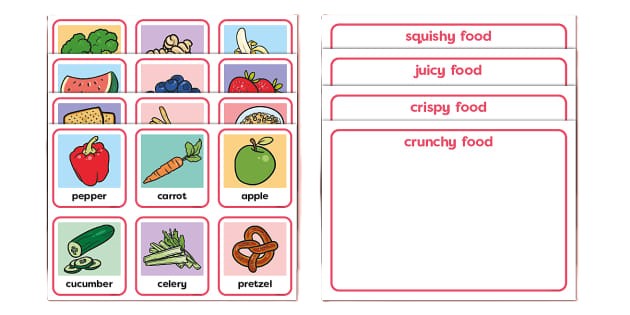
Sensory Exploration and Ratings Cards
For some children, food play can be a helpful first step. In a session, one young person used playdough to create different foods they had tried or wanted to try, imagining their taste and texture and even what it might be like if they enjoyed them. This allows children to engage with food concepts without pressure and supports imaginative, low-stress exploration.
Rating cards can be a useful tool to describe food textures and flavours, such as crunchy/soft, dry/wet, smooth/lumpy, and help children build their sensory language. We may also use rating scales, such as numbers, emojis, or smiley faces, to encourage moving away from “I love it” or “I hate it” thinking.
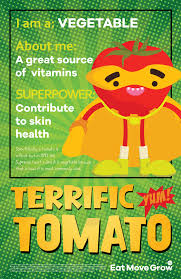
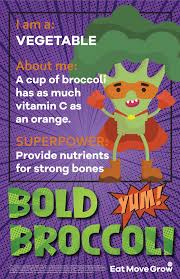
Superhero Foods
Some children enjoy learning about foods through a “superhero” lens. Together, we explore what makes certain foods powerful and what they do for the body, such as helping muscles grow strong, supporting energy levels, or protecting the immune system. By framing foods as superheroes with special powers, children can build curiosity and positive associations, shifting the focus away from fear and towards strength and nourishment.
How Parents and Carers Can Help
Parents and carers play a vital role in recovery. Supporting a child with ARFID may involve:
At First Steps ED, our person-centred approach includes face-to-face support, online sessions, psychotherapy, nutrition guidance, befriending, and workshops. We also provide guidance for parents and carers, because we have strong evidence that recovery works best when the whole family is supported.
There is no single “right” way to support a child with ARFID. Every child has unique needs, sensory sensitivities, and interests that influence how they experience food. By being flexible, creative, and responsive, we can help children build confidence, explore foods safely, and find joy in eating, one small step at a time.